Introduction
Anxiety and depression are two major mental health issues that impact millions of people worldwide. They may have a profound impact on a person’s quality of life, making it essential to find effective solutions for their treatment. While therapy and lifestyle changes play a vital role in managing these conditions, medicine can also be a valuable tool.
In the further lines of this blog, we will explore the causes, symptoms, and impact of anxiety and depression, the importance of medication in their treatment, review the top medicines available, provide guidance on choosing the proper medication, and offer tips for managing mental health alongside medicine. To dive into the depth of the topic, keep reading.
Understanding Anxiety and Depression: Causes, Symptoms, and Impact
Anxiety and depression are complex mental health disorders with multifaceted causes, symptoms, and far-reaching impacts on a person’s life.
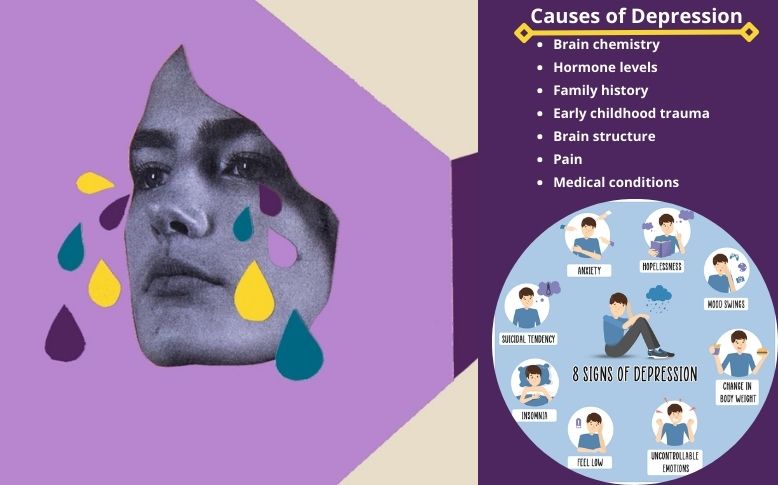
Causes of Anxiety and Depression
Genetic factors: A family history of these disorders can increase one’s risk.
Brain chemistry: Imbalances in neurotransmitters like serotonin and norepinephrine can contribute.
Environmental factors: Stress, trauma, abuse, or major life changes can trigger or exacerbate symptoms.
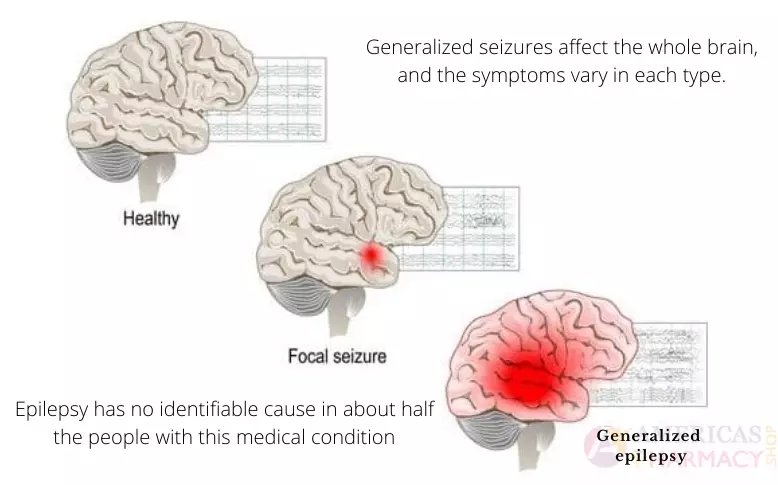
Medical conditions: Chronic illnesses and certain medicines may influence mental health.
Symptoms of Anxiety and Depression
- Anxiety symptoms include excessive worry, restlessness, and physical symptoms like rapid heartbeat.
- Depression symptoms often involve persistent sadness, fatigue, changes in appetite, and sleep disturbances.
- Both disorders may lead to irritability, difficulty concentrating, and social withdrawal.
Impact of Anxiety and Depression
Impaired daily functioning: Anxiety and depression can interfere with work, relationships, and daily tasks.
Physical health consequences: Chronic stress can lead to heart problems, weakened immunity, and more.
Increased risk of substance abuse: Few people turn to substances as a coping mechanism.
Suicidal thoughts and actions: In severe cases, these disorders can lead to life-threatening situations.
Importance of Medication in Treating Anxiety and Depression
Medication plays a critical role in treating anxiety and depression, mainly when symptoms are acute or resistant to other forms of therapy. While not a cure, these medicines can effectively alleviate symptoms, allowing people to better engage in therapeutic interventions and make necessary lifestyle changes.
Complementary to Therapy
- Medicine can be used alongside psychotherapy to provide a multi-pronged approach to treatment.
- Therapy helps address the underlying causes and provides coping strategies, while medicine manages symptoms.
Rapid Symptom Relief
- Medication can provide quick relief from severe symptoms, making it easier for people to function and engage in therapy.
- In some cases, medication can be a lifesaving intervention, especially when suicidal thoughts or actions are present.
Restoring Neurotransmitter Balance
- Antidepressants and anti-anxiety medicines work by regulating neurotransmitters rebalancing brain chemistry.
- This rebalancing helps reduce symptoms and improve overall well-being.
Reducing Relapse Risk
- Medicine can decrease the risk of relapse, helping people maintain mental health stability.
- It can be especially beneficial for those with recurrent or chronic forms of anxiety and depression.
Top Medications for Anxiety and Depression: A Comprehensive Review
There are several types of medications used for treating anxiety and depression. The choice of medicine depends on the specific diagnosis and individual response. Here, we will review some of the most commonly prescribed drugs for these conditions:
Therapy and lifestyle changes are vital components of treatment; medicines can also play a crucial role in managing these disorders. This comprehensive review explores some of the top medicines commonly prescribed for anxiety and depression.
SSRIs (Selective Serotonin Reuptake Inhibitors):
SSRIs like fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro) are often the first-line treatment for both anxiety disorders and depression. They work by boosting the levels of serotonin in the brain, which may improve mood and lower symptoms.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs):
Medications such as venlafaxine (Effexor) and duloxetine (Cymbalta) are SNRIs that target both serotonin and norepinephrine. They can be effective for people with depression or anxiety, primarily when SSRIs don’t provide sufficient relief.
Benzodiazepines:
Benzodiazepines like diazepam (Valium) and alprazolam (Xanax) are used to manage acute anxiety symptoms. However, they are generally prescribed for short-term use due to the risk of withdrawal and dependence.
Atypical Antidepressants:
Drugs like bupropion (Wellbutrin) and mirtazapine (Remeron) can be used when SSRIs or SNRIs are ineffective. They have different mechanisms of action and can be particularly useful for people with atypical depression or specific anxiety symptoms.
Tricyclic Antidepressants (TCAs):
TCAs, such as amitriptyline and imipramine, are older antidepressants that are sometimes used when other medications have not been effective. They can have more side effects and require careful monitoring.
Monoamine Oxidase Inhibitors (MAOIs):
MAOIs like phenelzine (Nardil) and tranylcypromine (Parnate) are rarely prescribed due to dietary restrictions and interactions with other medicines. However, they can be effective for treatment-resistant cases of depression.
It’s important to note that medication choice should be individualized, considering factors like the specific diagnosis, severity of symptoms, and potential side effects. Furthermore, the use of these medicines should be closely monitored by a healthcare expert to ensure safety and efficacy.
Combining medicine with therapy and lifestyle changes can offer a holistic approach to managing anxiety and depression, providing people with the best chance of improvement and recovery. Patients should always consult with their healthcare experts to determine the most suitable treatment plan for their unique needs.
How to Choose the Right Medication for Your Anxiety and Depression
Choosing the right medication for anxiety and depression requires careful consideration by both the person and their healthcare expert. There are various options for depression and anxiety medication. Here are some essential factors to keep in mind when making this critical decision:
Consult a Mental Health Professional
Begin by consulting with a psychiatrist or other mental health specialist who can make a precise diagnosis and recommend appropriate treatment.
Consider Diagnosis and Symptoms
The choice of medicine depends on the specific diagnosis (e.g., major depressive disorder, generalized anxiety disorder) and the severity of symptoms.
Individual Response
Medications can affect people differently. What works well for one person may not be effective for another. Be open to adjusting the treatment plan if needed.
Side Effects and Tolerability
You should discuss potential side effects with your healthcare expert. Some side effects may be intolerable, while others may be manageable.
Medication Interactions
You must inform your healthcare expert about all medications, including OTC drugs and supplements, to ensure there are no harmful interactions.
Potential for Dependency
With certain medicines, like benzodiazepines, there may be a risk of dependence. Be cautious and use these under close supervision.
Treatment Duration
Decide whether medication will be a short-term or long-term solution. Some people may only need medication for a specific period, while others may require ongoing treatment.
Lifestyle and Personal Preferences
You must consider your daily routine and lifestyle when choosing a medication. Some medications may be taken once a day, while others require multiple doses.
Regular Monitoring
Ongoing communication with your healthcare expert is essential. Daily check-ups and adjustments to your treatment plan may be necessary.
Tips for Managing Anxiety and Depression Alongside Medication
Here are some essential tips to help people effectively manage these conditions alongside their prescribed medications:
Therapy and Counseling:
Consider psychotherapy, such as cognitive-behavioral therapy (CBT) or mindfulness-based therapy, to learn coping strategies, address underlying issues, and gain emotional support.
Lifestyle Modifications:
You should prioritize regular exercise, a balanced diet, and adequate sleep. Physical activity can boost mood, and a healthy diet may have a positive impact on brain chemistry.
Stress Reduction Techniques:
You must practice relaxation techniques like progressive muscle relaxation, meditation, and deep breathing to lower stress and anxiety. These techniques can complement medication by promoting relaxation.
Social Support:
Maintain connections with friends and family. Social support can provide emotional validation and a sense of belonging, which is essential for mental well-being.
Mindfulness and Mind-Body Practices:
You should engage in mindfulness meditation or yoga, which can help improve self-awareness and emotional regulation.
Set Realistic Goals:
Break tasks into manageable steps and set achievable goals. This can help prevent feeling overwhelmed, a common trigger for anxiety and depression.
Avoid Alcohol and Substance Abuse:
Refrain from excessive alcohol or drug use, as these can exacerbate symptoms and interfere with medication effectiveness.
Regular Medication Monitoring:
Follow your healthcare expert’s advice for medication use, including dosages and scheduling. Keep them informed of any side effects or concerns.
Self-Care:
Make self-care a priority. You should engage in activities you enjoy and practice self-compassion. Take time for hobbies and relaxation.
Educate Yourself:
Learn about your condition and treatment options. Being informed can empower you to make better decisions about your mental health.
Remember that managing depression and anxiety is a personalized journey. It’s essential to work closely with a healthcare expert who can tailor your treatment plan to your specific needs, regularly assess your progress, and make necessary adjustments. Combining medication with these lifestyle and self-care strategies can provide a well-rounded approach to managing and improving mental health.
Conclusion
I hope you find this blog informative. We have mentioned anxiety and depression in the above section. Anxiety disorders and depression are challenging conditions that can impact a person’s life. While medication is not the sole solution, it can play a major role in managing symptoms and promoting well-being.
By understanding the causes, symptoms, and impact of these disorders, considering the available medications, and working closely with a healthcare expert to select the right treatment, people can effectively navigate their journey toward recovery. Remember that managing anxiety and depression is an ongoing process, and the combination of medication, therapy, and healthy lifestyle choices can help people lead fulfilling lives despite these challenges.
FAQs:
1- What are the common medications used to treat anxiety and depression?
Common medicines for anxiety and depression include Selective Serotonin Reuptake Inhibitors (SSRIs) like Prozac and Zoloft, Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) like Cymbalta, benzodiazepines like Xanax, antidepressants like Wellbutrin, tricyclic antidepressants (TCAs) like Elavil, and monoamine oxidase inhibitors (MAOIs) like Nardil. The choice of drug depends on your specific diagnosis and symptoms.
2- Are antidepressants and anti-anxiety drugs the same thing?
Antidepressants and anti-anxiety drugs are not the same but may have some overlap in their effects. Antidepressants are primarily used to treat depression, but some can also help with anxiety disorders. Anti-anxiety drugs, like benzodiazepines, are specifically designed to alleviate anxiety symptoms. You should consult your healthcare expert. They help you to determine the most suitable medicine for your condition.
3- How do I know if medication is the right choice for my anxiety and depression?
The decision to use medicine should be made in consultation with a mental health expert, such as a psychiatrist. Medication may be considered when symptoms are severe, persistent, or significantly impair daily functioning. It’s vital to consider your diagnosis, individual response, potential side effects, and overall treatment plan before starting medication.
4- What are the potential side effects of anxiety and depression medications?
The potential side effects of these medications vary depending on the type of drug. Common side effects may include nausea, insomnia, drowsiness, sexual dysfunction, weight changes, or increased blood pressure. It’s essential to discuss potential side effects with your healthcare expert and monitor your response to the medicine.
5-Can I take medication for anxiety and depression alongside therapy?
Yes, medication can be taken alongside therapy, and this combination is often recommended for comprehensive treatment. Therapy, such as CBT, can help people address the major causes of their condition and develop coping strategies. Medicine can provide relief from symptoms, making it easier to engage effectively in therapy. It’s a synergistic approach that can lead to better outcomes for many people.